What is Visual Impairment?
“Visual impairment” is loss of vision that can never be fully corrected by eyeglasses or contact lenses.
How Common is Visual Impairment?
According to the NHS, more than 2 million people in the United Kingdom live with a visual impairment. Of those 2 million, around 340,000 are registered as blind or visually impaired.
Visual Impairment – a checkup is essential!
Because we rely so heavily on our vision and because visual impairment is so common, it is recommended that everyone see an eye doctor at least every two years to look for signs of low vision.
If someone already has a visual impairment, regular vision tests are even more important to monitor for further changes in the eyes to minimise progression.
What Causes Visual Impairment
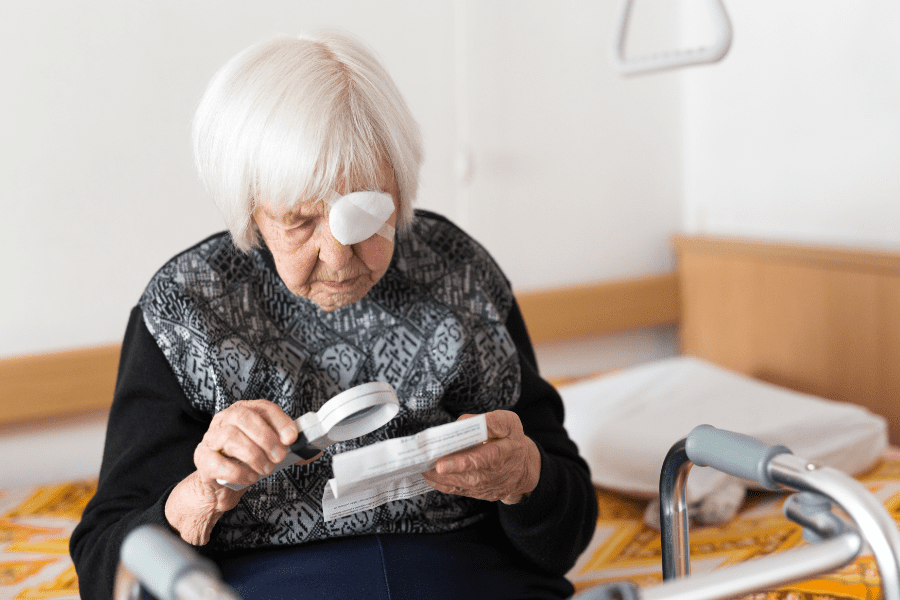
In most cases, visual impairment is due to diseases which develop with age. About 80% of visually impaired people are over the age of 65. Visual impairment isn’t inevitable with ageing, however as many common diseases can be treated or prevented. Age-related macular degeneration (AMD) is the most important condition, in which the macula loses its normal function.
Cataract is a common condition in which cloudy spots form in the lenses of the eye. Glaucoma, which can develop gradually without early symptoms, occurs when fluid pressure builds up inside the eye, damaging the optic nerve. Diabetic retinopathy occurs when blood vessels at the back of the eye become damaged due to high blood sugar levels in diabetics.
Some common causes of vision loss in elderly patients are:
Age-Related Macular Degeneration
Age-related macular degeneration (AMD) is the most common cause of vision loss in people over the age of 65. AMD is characterised by degeneration of the macula, the area of the retina responsible for central vision.
Risk factors for AMD include advancing age, a family history of AMD, and cardiovascular risk factors such as hypertension and cigarette smoking. We can divide AMD into two categories: non-exudative or “dry” AMD and exudative or “wet” AMD.
Age-Related Macular Degeneration.
Fundus photographs demonstrate age-related macular degeneration.
Glaucoma
Glaucoma comprises a group of disorders characterised by glaucomatous optic nerve damage and visual field loss. It is a significant cause of blindness in the UK.
The most prevalent form of glaucoma is primary open-angle glaucoma.
Glaucoma. Fundus photograph demonstrates glaucomatous optic disc cupping and pallor,
in a patient with associated elevation of intraocular pressure and visual field loss.
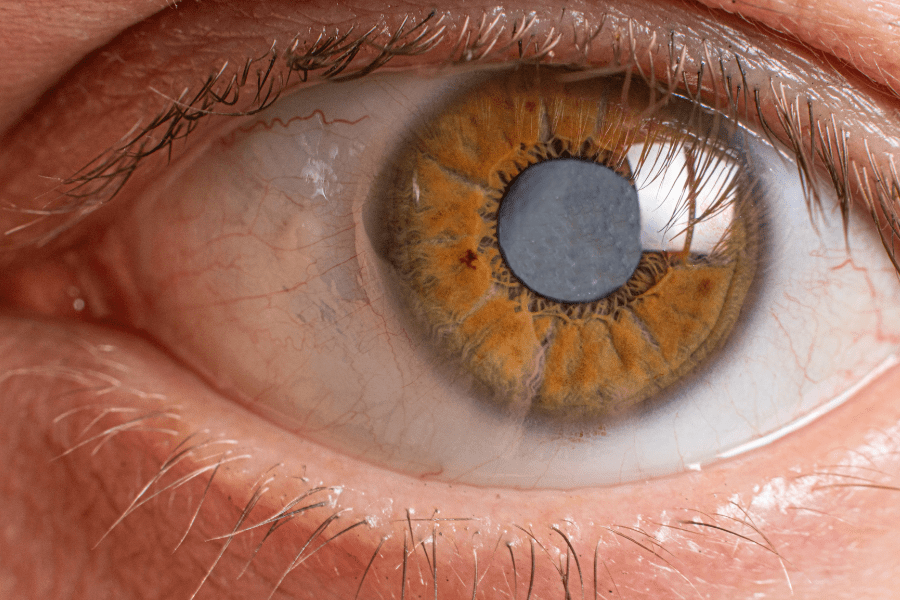
Cataract
Cataract is a common cause of vision impairment in the elderly and the most common cause of blindness.
Exposure to ultraviolet light may contribute to the progression of cataract formation.
Cataract. A slit lamp image shows a pronounced lens opacity in the left eye.
The patient complained of a slowly progressive, painless loss of vision.
Diabetic Retinopathy
Diabetic retinopathy is the most common cause of new blindness. It is also an important cause of vision morbidity in the elderly population. The prevalence of diabetic retinopathy increases with the duration of diabetes.
However, even at the time of diagnosis or during the early years of diabetes, the elderly may exhibit significant diabetic retinopathy. We can divide Diabetic retinopathy into two categories: non-proliferative and proliferative retinopathy.
Diabetic retinopathy. Fundus photograph of a 70-year-old man with a seven-year history of diabetes. Examination shows non-proliferative diabetic retinopathy with intraretinal haemorrhages, microaneurysms, lipid exudate, and macular edema.
Risk
It can also be very useful to request a fall sensor if you are a careline service user. A fall sensor detects when you have fallen and activates your personal alarm. If you can’t reach your pendant, you will get immediate assistance from your care team.
Please check out our blogs for more useful information like the one in this article.